Introduction
As discussed in previous chapters, periodontal infections have been shown to act as a risk factor for various systemic diseases. With increasing research in the field of periodontal medicine, more evidence is coming into picture, demonstrating the relationship between periodontal diseases and various systemic conditions. The relationship between periodontal diseases and pulmonary infections is well established. In the following discussion, we shall try to understand various aspects of the relationship between periodontal and pulmonary diseases. The two most investigated types of respiratory diseases for their association with periodontitis include: acute, most commonly pneumonia, and chronic, focused on chronic obstructive pulmonary disease (COPD) that includes chronic bronchitis and emphysema.
| Chronic lung diseases: Chronic obstructive pulmonary disease (COPD) | |
|---|---|
| Chronic bronchitis | • Excessive tracheobronchial mucous production with a chronic cough lasting >3 months over 2 consecutive years. • Chronic and productive cough. • Copious sputum. • Mild dyspnea. • Frequent respiratory infections. |
| Emphysema | • Distention of air spaces due to destruction. • Cough not prominent, scanty sputum, severe dyspnea. • Few respiratory infections. • Some symptoms frequently overlap with those of chronic bronchitis (emphysema can only be definitively diagnosed through autopsy). |
| Acute lung infections: Pneumonia | |
| Community-acquired pneumonia (CAP) | • Most common form of pneumonia. • Occurs outside of hospitals or other healthcare facilities. • Inhalation of infections aerosols; spread of infections from extrapulmonary sources of infection. • Common pathogens: Streptococcus pneumoniae and Haemophilus influenza. |
| Hospital acquired pneumonia (Nosocomial) (HAP) | • Inhalation of infections aerosols; spread of infections from extrapulmonary sources of infection. • Usually more severe than CAP due to compromised host or more virulent/antibiotic-resistant pathogens. • Common pathogens: Staphylococcus aureus (methicillin-susceptible and resistant), and Enterobacter. |
| Ventilator-associated pneumonia (VAP) | • Type of HAP occurring in mechanically ventilated patients. • Spread of infections from extrapulmonary sources of infection. • Most common hospital-acquired infection. • Common pathogens: P aeruginosa, Staphylococcus aureus, including methicillin-susceptible S. aureus (MSSA) and methicillin-resistant S. aureus (MRSA), Klebsiella pneumoniae. |
| Aspiration pneumonia | • Aspiration of oropharyngeal secretions, food or gastric contents. • Pus formation in a cavity of the lung can lead to lung abscess. |
Chronic obstructive pulmonary disease (COPD)
COPD is a type of obstructive lung disease characterized by long-term breathing problems and poor airflow. The main symptoms include shortness of breath and cough with sputum production. COPD is a progressive disease, that is, it typically worsens over time. It is a major cause of morbidity and mortality worldwide. It is the sixth leading cause of deaths. It is important to emphasize here that COPD is a generic term that is defined by the presence of airflow obstruction. It consists of several pathological subtypes, such as emphysema, small airways disease and chronic bronchitis, that are distinct entities although often combined in a single patient.
Chronic bronchitis results from irritation to the bronchial airway that increases the proportion of mucous secreting cells within the airway epithelium which secretes excessive tracheobronchial secretion. This secretion causes cough with expectoration for at least 3 months of the year over two consecutive years 1. Emphysema results from distention of air spaces distal to terminal bronchiole with the destruction of alveolar septa. One major complication of COPD is the occurrence of “exacerbation” periods during which ……… Contents available in the book…….. Contents available in the book…….. Contents available in the book…….. Contents available in the book…….. Contents available in the book……..
The infection in lower respiratory tract occurs primarily by the inhalation of contaminated aerosol droplets or aspiration of oral secretions contaminated by microorganisms. One of the most critical steps in lower respiratory tract infection by these microorganisms is their attachment and colonization on oropharyngeal mucosal surfaces and subsequent shedding of these bacteria into contagious secretions that ultimately contaminate the lower respiratory tree 4, 5. If the host immune response is unable to eliminate these bacteria, they subsequently proliferate and colonize in the respiratory tract causing tissue destruction 6-8.
The microorganisms inhabiting oral cavity have been implicated as important causative factors for respiratory diseases. It has been observed that severe anaerobic respiratory infections may result from the aspiration of salivary secretions, especially in patients with periodontal diseases 5, 9. Many studies done on patients in medical intensive care units (MICU) have demonstrated that patients admitted in MICU have more prevalence of respiratory pathogen colonization on the teeth and oral mucosa than do the age and gender-matched outpatients 10-12. Many researchers have suggested that poor oral hygiene may act as a reservoir for respiratory infections. The precise underlying mechanism involved in respiratory infection originating from the oral cavity has not been described. Many studies have described a weak association between periodontal disease and COPD 13-15.
In a case-control study, a significant association between periodontal disease and airway obstruction, particularly in former smokers was found 16. Another study demonstrated that dental plaque in patients with chronic lung diseases often serves as a reservoir of bacteria known to cause nosocomial pneumonia in susceptible individuals 17. Wang et al. (2009) 18 in a study, evaluated ……… Contents available in the book…….. Contents available in the book…….. Contents available in the book…….. Contents available in the book…….. Contents available in the book……..
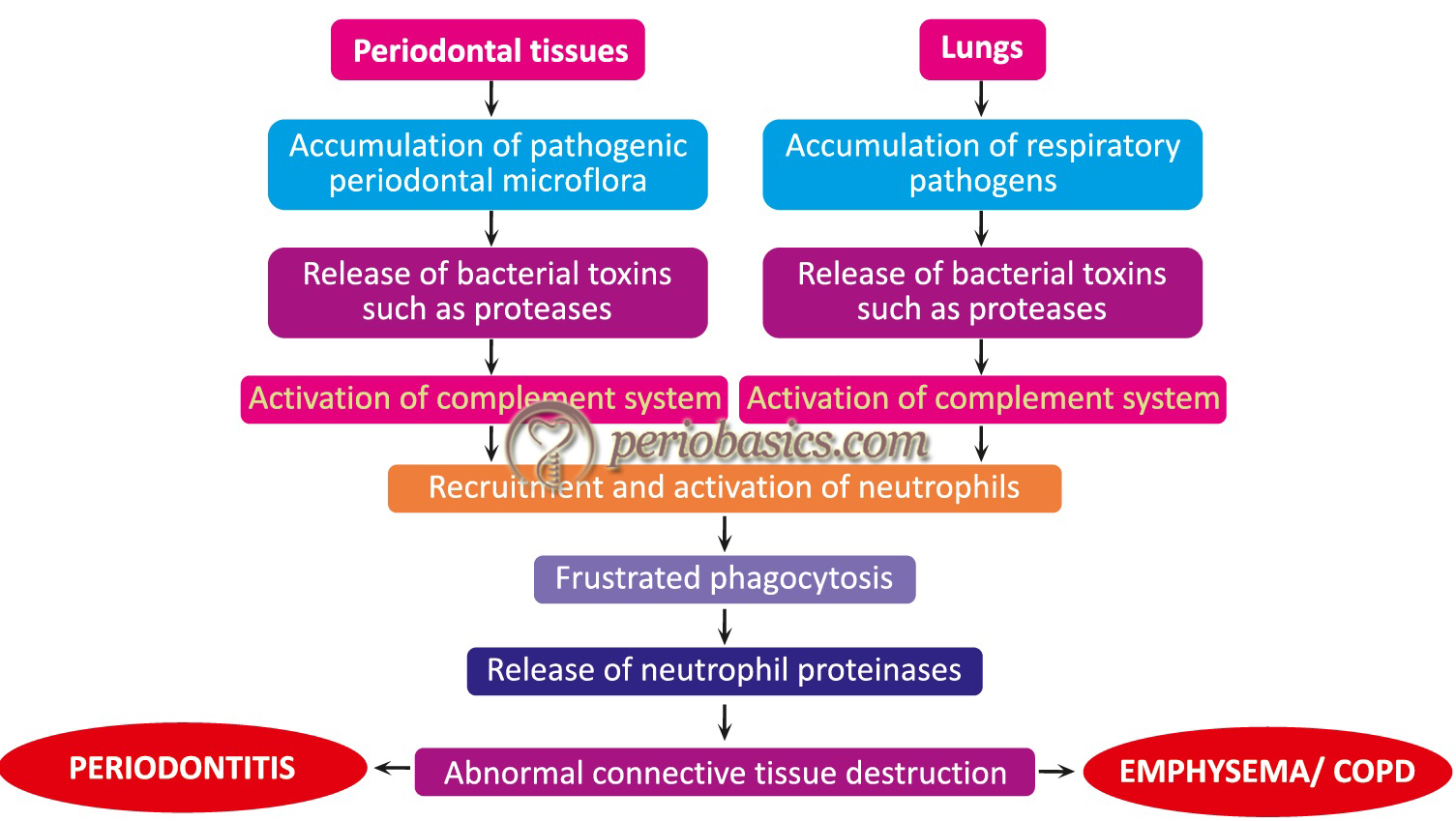
Proposed mechanisms of association of oral bacteria in the pathogenesis of respiratory infection
Four mechanisms have been proposed to explain the association of oral bacteria in the pathogenesis of respiratory infection by Scannapieco and Genco (1999) 19. These are,
- By aspiration of oral pathogens in the lungs.
- By action of periodontal disease-associated enzymes in saliva on the mucosal surface to promote adhesion and colonization by respiratory pathogens.
- By periodontal diseases associated enzymes, which may destroy protective salivary pellicles.
- By cytokines originating from periodontal tissues, which may alter respiratory epithelium to promote infection by respiratory pathogens.
Aspiration of oral pathogens in the lungs:
Various studies have identified the oral bacteria in the sputum of patients with bacterial pneumonia 20-22. It is a well-established fact that various oral bacteria, specifically, anaerobic bacteria, primarily derived from periodontal pockets may get aspirated and may cause respiratory infections. Studies have shown the presence of oral bacteria, such as A. actinomycetemcomitans, Actinomyces israelii, Capnocytophaga species, Eikenella corrodens, and others, in infected sputum and lung abscesses 23. These pathogens may get access to the lower respiratory tract and cause respiratory diseases. If the host immune response is able to eliminate these organisms, the disease stops and if not the disease progresses.
Action of periodontal disease-associated enzymes in saliva on the mucosal surface:
Studies have suggested that mucosal alterations promote bacterial adhesion by respiratory pathogens. It is a well-established fact that in periodontal disease the levels of salivary hydrolytic enzymes are increased. It has been proposed that hydrolytic enzymes from saliva alter fibronectin thereby exposing the mucosal receptors for bacterial adhesion. It has been shown that trypsin treatment of epithelial cells from non-colonized patients in vitro resulted in increased adhesion by respiratory pathogens 24. The enzymatic activity of saliva is increased in patients with poor oral hygiene and periodontal diseases. In a study, it was demonstrated that the ability of saliva to degrade fibronectin increases with poor oral hygiene 25. Many studies have reported that ……… Contents available in the book…….. Contents available in the book…….. Contents available in the book…….. Contents available in the book…….. Contents available in the book……..
Enzymatic degradation of protective salivary pellicles:
The hydrolytic enzymes produced by various periodontopathogens degrade the protective salivary molecules such as salivary mucins which coat the bacteria for their clearance from oral cavity 32. It has been shown that the adhesion of H. influenzae to mucosal surfaces is mediated by sialic acid residues 33, 34. The enzymes secreted by various oral bacteria have the ability to destroy the protective domains of the host secretory components such as mucins. Once these protective domains are degraded, the bacteria can easily colonize on the mucosal surfaces.
Cytokine-mediated alterations in respiratory epithelium:
It is a well-established fact that oral pathogens stimulate various cells in periodontal tissues, including epithelial cells, endothelial cells, fibroblasts, and T-cells. These cells, in turn, secrete various cytokines, which are mediators of inflammation. These cytokines include IL-1α, IL-1β, TNF-α, IL-6, and IL-8. These cytokines participate in alteration the expression of cell ……… Contents available in the book…….. Contents available in the book…….. Contents available in the book…….. Contents available in the book…….. Contents available in the book……..
Pneumonia
Pneumonia is the inflammation of one or both lungs, with dense areas of inflammation. It is usually, but not always caused by microbial infection. The infection may be bacterial, viral, fungal, or parasitic. Symptoms may include fever, chills, cough with sputum production, chest pain, and shortness of breath. It can be a life-threatening infection, especially in the elderly and immunocompromised patient. Pneumonia can be broadly classified into two types: community- or hospital-acquired (nosocomial). Community-acquired pneumonia is an infection that is acquired outside of the healthcare system (including hospitals, nursing homes, outpatient clinics, or any other healthcare facility). It is the most common type of pneumonia and generally presents as an acute infection, with symptoms appearing over the course of hours or days. Streptococcus pneumoniae is the leading cause of community-acquired pneumonia, responsible for 20% to 60% of all cases. Other microorganisms associated with this disease are Haemophilus influenza, Staphylococcus aureus, Ligonella pneumophila, Chlamydia pneumoniae, Mycoplasma pneumonia, and several viruses 37.
Hospital-acquired pneumonia is a lung infection obtained during a hospital stay. This type of pneumonia is difficult to treat because usually, the patient has lowered immunity and the presence of resistant strains. Infection can occur through inhalation of airborne organisms or through contact with contaminated healthcare workers. Hospital-acquired pneumonia is also prevalent in patients who require a ventilator for breathing assistance. Ventilator tubes or other tubes that open a patient’s throat provide a direct point of access for airborne bacteria and viruses to enter the lungs. The microorganisms involved in nosocomial pneumonia are ……… Contents available in the book…….. Contents available in the book…….. Contents available in the book…….. Contents available in the book…….. Contents available in the book……..
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
Role of oral pathogens in the pathogenesis of pneumonia:
The structure of the lungs is such that it provides a large area for gaseous exchange. After trachea, the bronchi subdivide further several times, and the smaller subdivisions of the bronchial tubes are called bronchioles. At the end of the airway tree are the pulmonary acini including respiratory bronchioles, alveolar ducts, and air sacs or alveoli, that are the destination of inhaled air. A human lung contains about 30000 acini, each with a diameter of 3.6 mm and containing about 10000 alveoli. The alveoli are the final branchings of the respiratory tree and act as the primary gas exchange units of the lung. The gas-blood barrier between the alveolar space and the pulmonary capillaries is extremely thin, allowing for rapid gas exchange.
In spite of the fact that the upper respiratory tract is heavily contaminated, the lower respiratory tract is usually sterile. The primary reasons for the sterility of lower respiratory tract are intact cough reflexes, the action of tracheobronchial secretions and mucociliary transport of inhaled microorganisms and particulate material from the lower respiratory tract to the oropharynx, and defense cells 9, 41. Various defense factors that coat the pulmonary epithelium include fibronectin, complement, and immunoglobulins, etc. Furthermore, lungs contain resident phagocytes which act as antigen-presenting cells.
Proposed mechanisms involved in the contamination of lower respiratory tract
Scannapieco and Mylotte (1996) 11 Proposed four possible mechanisms to explain the contamination of the lower respiratory tract,
- Aspiration of oropharyngeal contents;
- Inhalation of infectious aerosols;
- Spread of infection from contiguous sites and
- Hematogenous spread from extrapulmonary sites of infection (e.g., translocation from the gastrointestinal tract).
As previously discussed in COPD, aspiration of oro-pharyngeal contents and inhalation of infected aerosols are important causes of respiratory infections. Various putative pathogens like S. pneumoniae, Staphylococcus pyogenes, M. pneumoniae, and H. influenzae can colonize the oropharynx and be aspirated into the lower airways. It has been observed that ……… Contents available in the book…….. Contents available in the book…….. Contents available in the book…….. Contents available in the book…….. Contents available in the book……..
The aspiration of the oral contents is more common with patients who have impaired consciousness (e.g., alcoholics, drug abusers, epileptics), those having chronic swallowing disorders, or those having mechanical interventions such as nasogastric or endotracheal tubes 44, 45.
Oral bacteria causing pneumonia
Various case reports have demonstrated that oral pathogens such as Aggregatibacter actinomycetemcomitans 46, Actinomyces israelii 47, 48, Capnocytophaga species 49, Eikenella corrodens 50, Prevotella intermedia, and Streptococcus constellatus 43 are involved in causing pneumonia. In a review, Scannapieco (2006) 51 stated that the mouth can be colonized by respiratory pathogens and serve as a reservoir for these organisms. The author suggested oral interventions aimed at controlling or reducing oral biofilms can reduce the risk of pneumonia in high-risk populations.
It should be remembered here that many of the oral bacteria are not identified using conventional cultivation methods. To identify them molecular detection techniques need to be employed. In a recent study employing 16S ribosomal RNA gene identification technique, the broncho-alveolar lavage specimens, obtained from community-acquired pneumonia patients, were analyzed. The authors concluded that anaerobes and oral bacteria are more frequently detected in patients with community-acquired pneumonia than previously believed and it is possible that these bacteria may play more important roles in community-acquired pneumonia 52. A study was conducted in Japan 53, where 417 patients were randomly assigned to an oral care group or a no oral care group. In the oral care group, nurses or caregivers cleaned the patients’ teeth by toothbrush after each meal and swabbing ……… Contents available in the book…….. Contents available in the book…….. Contents available in the book…….. Contents available in the book…….. Contents available in the book……..
Conclusion
From the above discussion, it is clear that poor oral health may play an important role in the pathogenesis of respiratory infection. The colonization of the respiratory tract with various periodontopathogens may result in respiratory diseases such as bacterial pneumonia. These findings are especially applicable to hospitalized patients in which the immunity is low and in patients on external respiratory support like ventilators. Furthermore, contaminated aerosols may also cause respiratory infections. Adequate maintenance of oral hygiene in these patients may reduce the chances of pneumonia by reducing the bacterial load in the oral cavity.
References
References are available in the hard-copy of the website.
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.

